What is breast reconstruction?
Breast reconstruction is a surgical procedure or series of procedures performed to rebuild or restore the shape, size, symmetry, and appearance of a breast or breasts following a mastectomy (surgical removal of the breast) or lumpectomy (partial removal of the breast) due to breast cancer or other medical conditions. Breast reconstruction aims to recreate a natural-looking breast mound to help restore a woman's sense of wholeness and femininity after breast surgery.
Why do women get breast reconstruction?
Women may choose to undergo breast reconstruction for various reasons, including:
- Restoring body symmetry: Breast reconstruction helps restore symmetry between the breasts, particularly following a mastectomy or lumpectomy for breast cancer treatment. This can improve body image and self-confidence.
- Improving psychological well-being: Breast reconstruction can have a positive impact on a woman's psychological well-being, helping her feel more whole, feminine, and confident after undergoing breast cancer surgery.
- Enhancing quality of life: For many women, breast reconstruction plays a significant role in improving their quality of life by allowing them to feel more comfortable in their bodies and clothing choices.
- Sense of normalcy: Breast reconstruction can help women regain a sense of normalcy and femininity after the physical changes resulting from breast cancer treatment.
- Avoiding external prosthetics: Breast reconstruction provides an alternative to external breast prosthetics, offering a more permanent and natural-looking solution.
- Personal choice: Some women choose breast reconstruction simply because they desire to restore their breast shape and size for personal reasons and aesthetic preferences.
Ultimately, the decision to undergo breast reconstruction is personal and varies for each individual. By discussing their options with a plastic surgeon specializing in breast reconstruction, women can explore the available techniques, understand the benefits and risks, and make an informed decision based on their medical needs, preferences, and goals.
Who are the ideal candidates?
Ideal candidates for breast reconstruction are typically women who have undergone a mastectomy or lumpectomy for breast cancer treatment or prevention and are in overall good health. Candidates for breast reconstruction may include:
- Women with breast cancer: Women who have been diagnosed with breast cancer and have undergone a mastectomy or lumpectomy as part of their treatment plan.
- Healthy individuals: Candidates should be in good overall health and free from medical conditions that may increase the risks associated with surgery and anesthesia.
- Realistic expectations: Candidates should have realistic expectations about the outcomes of breast reconstruction and understand that the results may vary based on individual factors.
- Non-smokers: It is generally recommended that candidates be non-smokers or willing to quit smoking before and after surgery to promote proper healing and reduce the risk of complications.
- Emotionally ready: Candidates should be emotionally prepared for the physical and emotional aspects of breast reconstruction, as the process may involve multiple surgeries and a period of recovery.
- Informed decision-making: Candidates should be actively involved in the decision-making process, understanding the different reconstruction options, potential risks, benefits, and alternatives available.
- Support system: Having a strong support system in place, including family, friends, and healthcare providers, can be beneficial for candidates undergoing breast reconstruction.
It is essential for women considering breast reconstruction to consult with a board-certified plastic surgeon specializing in breast reconstruction to evaluate their individual circumstances, discuss their goals and concerns, and determine the most appropriate reconstruction approach based on their medical history and preferences. A thorough evaluation and open communication with the surgeon can help ensure the best possible outcomes for breast reconstruction surgery.
Different breast reconstruction techniques
There are several breast reconstruction techniques available, each offering unique benefits and considerations. Some common breast reconstruction techniques include:
- Implant-based reconstruction:
- Direct-to-implant reconstruction
- Two-stage reconstruction
- Autologous tissue reconstruction:
- TRAM flap (Transverse Rectus Abdominis Myocutaneous flap)
- Latissimus dorsi flap
- DIEP flap (Deep Inferior Epigastric Perforator flap)
- SGAP flap (Superior Gluteal Artery Perforator flap) and IGAP flap (Inferior Gluteal Artery Perforator flap
- Combination reconstruction
- Combines implant-based techniques with autologous tissue reconstruction to achieve optimal results, such as using an implant in combination with a flap procedure.
- Nipple reconstruction
- Involves creating a new nipple and areola using local tissue or tattooing techniques to provide a natural-looking appearance.
- Revision surgery
- Additional procedures may be performed to refine the reconstructed breast shape and symmetry or address any complications that may arise.
The choice of breast reconstruction technique depends on various factors, including the patient's anatomy, medical history, personal preferences, and the recommendation of the plastic surgeon. It is crucial for individuals considering breast reconstruction to discuss their options with a qualified plastic surgeon specializing in breast reconstruction to determine the most suitable technique based on their individual needs and goals.
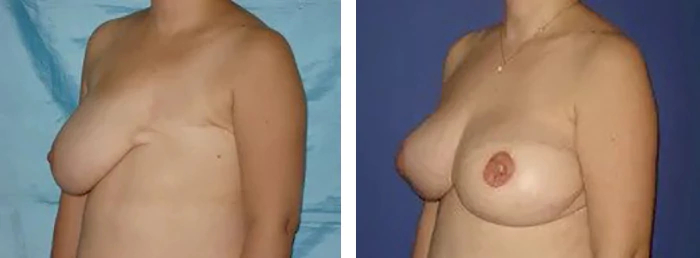
Breast reconstruction using implants
Breast reconstruction using implants, also known as implant-based breast reconstruction, is a common technique that involves the use of saline or silicone implants to recreate the breast mound after a mastectomy or lumpectomy. The process of breast reconstruction using implants typically involves the following steps:
- Tissue expansion: If a tissue expander is used, it is placed beneath the chest muscle during the initial surgery and gradually filled with saline solution over several weeks to stretch the skin and muscle.
- Implant placement: Once the desired expansion is achieved, the tissue expander is replaced with a permanent silicone or saline implant during a second surgery.
- Nipple and areola reconstruction: After the breast mound is reconstructed, the nipple and areola can be recreated through additional procedures, such as nipple reconstruction or tattooing.
Implant-based breast reconstruction offers several benefits, including:
- Minimal surgical complexity: Implant-based reconstruction is generally less invasive and requires fewer surgical incisions compared to autologous tissue reconstruction.
- Shorter recovery time: Patients undergoing implant-based reconstruction may experience a shorter recovery period compared to procedures using autologous tissue, as there is no additional donor site to heal.
- Customizable results: Implants come in various shapes, sizes, and profiles, allowing plastic surgeons to customize the reconstruction to achieve the desired breast shape and size.
- Single-stage reconstruction: In some cases, direct-to-implant reconstruction can be performed in a single surgery, eliminating the need for tissue expanders and additional procedures.
- Less donor site morbidity: Unlike autologous tissue reconstruction, implant-based reconstruction does not require tissue harvesting from other areas of the body, reducing donor site complications.
It is essential for individuals considering breast reconstruction with implants to consult with a board-certified plastic surgeon specializing in breast reconstruction to discuss the options available, understand the benefits and risks of the procedure, and determine the most suitable approach based on their individual needs and preferences. Regular follow-up appointments and monitoring are necessary to ensure the long-term success and satisfaction of implant-based breast reconstruction.
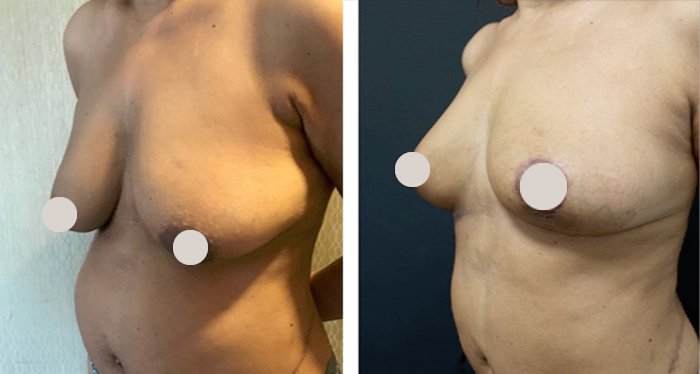
Autologous tissue reconstruction:
Autologous tissue reconstruction, also known as autologous flap reconstruction, is a breast reconstruction technique that uses the patient's own tissue from another part of the body to recreate the breast mound after a mastectomy. Some common types of autologous tissue reconstruction techniques include:
- TRAM flap (Transverse Rectus Abdominis Myocutaneous flap): Uses tissue from the abdomen, including skin, fat, and sometimes muscle, to reconstruct the breast.
- DIEP flap (Deep Inferior Epigastric Perforator flap): Similar to the TRAM flap but spares the abdominal muscle, reducing the risk of abdominal wall weakness.
- Latissimus dorsi flap: Utilizes muscle, skin, and fat from the back to reconstruct the breast mound. In some cases, an implant may be used in conjunction with the flap.
- Gluteal flaps (SGAP and IGAP): Use tissue from the buttocks to reconstruct the breast, offering an alternative donor site for autologous reconstruction.
This approach offers several advantages, including:
- Natural look and feel: Autologous tissue reconstruction can result in a breast that looks and feels more natural because it uses the patient's own skin, fat, and sometimes muscle to reconstruct the breast mound.
- Long-term durability: The reconstructed breast using autologous tissue is considered to be more durable and less prone to complications such as implant rupture or capsular contracture over the long term.
- Improved aesthetics: Autologous tissue reconstruction allows for a more customized reconstruction that can closely match the size, shape, and contour of the natural breast.
- Potential for simultaneous procedures: In some cases, autologous tissue reconstruction can be combined with procedures like a tummy tuck (abdominoplasty) or thigh lift, leading to improved body contouring.
- Avoidance of implants: For patients who prefer not to have breast implants or have concerns about implant-related complications, autologous tissue reconstruction can be an alternative option.
Autologous tissue reconstruction is a complex procedure that requires meticulous surgical planning and expertise. Patients considering this technique should consult with a board-certified plastic surgeon specializing in autologous tissue reconstruction to discuss the options available, understand the benefits and risks of the procedure, and determine the most suitable approach based on their individual needs and goals. Regular follow-up care and monitoring are essential to ensure the long-term success and satisfaction of autologous tissue breast reconstruction.
How do I prepare for breast reconstruction surgery?
Preparing for breast reconstruction surgery involves several important steps to ensure a successful procedure and smooth recovery. Here are some general guidelines on how to prepare for breast reconstruction surgery:
- Consultation with a plastic surgeon: Schedule a consultation with a board-certified plastic surgeon specializing in breast reconstruction to discuss your options, goals, and medical history. Make sure to ask questions, express any concerns, and understand the details of the procedure.
- Medical evaluation: Your plastic surgeon will perform a thorough medical evaluation to assess your overall health and identify any potential risk factors that may affect the surgery or recovery process.
- Quit smoking: If you are a smoker, it is advisable to quit smoking several weeks before surgery to reduce the risk of complications and promote better healing.
- Medication review: Inform your surgeon about any medications, supplements, or herbal remedies you are currently taking, as some may need to be adjusted or temporarily stopped before surgery.
- Follow preoperative instructions: Your surgeon will provide specific preoperative instructions, which may include guidelines on eating, drinking, medications to avoid, and showering with antibacterial soap before surgery.
- Arrange for transportation: Plan for someone to drive you to and from the surgical facility on the day of surgery, as you may not be able to drive yourself after the procedure.
- Prepare your recovery space: Set up a comfortable recovery area at home with essential items such as loose-fitting clothing, extra pillows for support, medications, and any recommended postoperative supplies.
- Arrange for support: Arrange for a support system to assist you during the initial recovery period, including help with daily activities, transportation, and emotional support.
- Follow fasting guidelines: Your surgeon will provide fasting instructions before surgery to reduce the risk of complications related to anesthesia.
- Stay hydrated: Maintain good hydration in the days leading up to surgery and follow any specific guidelines provided by your surgeon.
It is essential to closely follow your surgeon's instructions and recommendations to prepare effectively for breast reconstruction surgery. By taking the necessary steps to prepare physically, mentally, and emotionally, you can help optimize the outcome of the procedure and facilitate a smoother recovery process.
What to expect on the surgery day
On the day of your breast reconstruction surgery, you can expect the following general process and events:
- Arrival at the surgical facility: You will arrive at the surgical facility at the scheduled time. Check in with the receptionist or nursing staff, who will guide you through the preoperative process.
- Preoperative preparation: You will be taken to a preoperative area where you will change into a surgical gown. A nurse or medical staff member will review your medical history, check vital signs, start an IV line for fluids and medications, and answer any last-minute questions you may have.
- Meeting with the anesthesiologist: An anesthesiologist will meet with you to discuss the type of anesthesia that will be administered during surgery and address any concerns you may have. They will monitor your condition throughout the procedure.
- Surgical markings: Your plastic surgeon will visit you before the surgery to make surgical markings on your chest and discuss the surgical plan, including the type of reconstruction technique to be performed.
- Operating room transfer: When it is time for your surgery, you will be transferred to the operating room. The operating room staff will assist you onto the operating table and ensure you are comfortable before the procedure begins.
- Surgery: The breast reconstruction surgery will be performed according to the predetermined surgical plan. The length of the surgery will depend on the complexity of the reconstruction technique chosen.
- Recovery room: After the surgery is completed, you will be taken to the recovery room, where you will be closely monitored as you wake up from anesthesia. The nursing staff will manage any discomfort and monitor your vital signs.
- Postoperative care: Once you are awake and stable, you will be transferred to a postoperative recovery area. The nursing staff will continue to monitor your condition, provide pain management as needed, and ensure your comfort.
- Discharge or hospital admission: Depending on the type of reconstruction and your surgeon's recommendations, you may be discharged home on the same day of surgery or kept overnight for observation.
- Follow-up instructions: Before leaving the surgical facility, your surgeon will provide postoperative instructions, including wound care, activity restrictions, pain management, and follow-up appointments.
It is essential to have a clear understanding of what to expect on the day of your breast reconstruction surgery by discussing the process with your surgical team beforehand. By being well-prepared and following your surgeon's guidance, you can help ensure a successful surgery and a smooth recovery.
Breast reconstruction recovery
The recovery process after breast reconstruction surgery can vary depending on the type of reconstruction technique used, individual healing capacity, and overall health. Here are some general guidelines on what to expect during the breast reconstruction recovery period:
- Immediate postoperative period
- Pain management: You may experience pain, swelling, and discomfort in the days following surgery. Your surgeon will prescribe pain medications to manage postoperative pain.
- Drains: If surgical drains were placed during the procedure, they will typically remain in place for a few days to collect excess fluid and reduce swelling. Your surgeon will provide instructions on drain care and when they can be removed.
- Compression garments: You may be required to wear a surgical bra or compression garment to support the reconstructed breast and minimize swelling.
- Activity restrictions: Your surgeon will provide guidelines on physical activity restrictions, including lifting, bending, and strenuous exercise, to promote proper healing.
- Recovery timeline
- First week: During the initial week post-surgery, focus on resting, following wound care instructions, and attending any follow-up appointments with your surgeon.
- 2-6 weeks: As you progress through the recovery process, you may gradually resume light activities and return to work, depending on your surgeon's recommendations.
- 6 weeks and beyond: Full recovery from breast reconstruction surgery can take several weeks to months. Your surgeon will advise you on when it is safe to resume normal activities, exercise, and daily routines.
- Wound care
- Incision care: Follow your surgeon's instructions for caring for incision sites, including keeping them clean and dry, changing dressings as needed, and monitoring for signs of infection.
- Scar management: Your surgeon may recommend scar massage, silicone gel sheets, or other scar management techniques to promote optimal healing and minimize scar visibility.
- Emotional support
- Breast reconstruction surgery can have emotional implications, and it is essential to seek support from loved ones, support groups, or mental health professionals if needed.
- Follow-up appointments
- Regular follow-up appointments with your plastic surgeon are crucial to monitor your healing progress, address any concerns, and ensure the long-term success of your breast reconstruction.
It is essential to communicate openly with your surgical team, follow postoperative instructions diligently, and be patient with the recovery process. By taking care of yourself and following your surgeon's guidance, you can help promote a smooth and successful recovery after breast reconstruction surgery.
Potential risks and complications
Breast reconstruction surgery, like any surgical procedure, carries inherent risks and potential complications. It is essential to understand these risks and discuss them with your plastic surgeon before undergoing surgery. Here are some common risks and complications associated with breast reconstruction surgery:
- General surgical risks
- Bleeding: Excessive bleeding during or after surgery may require additional interventions.
- Infection: Infections at the surgical site can occur and may require antibiotics or additional treatment.
- Anesthesia risks: Adverse reactions to anesthesia, though rare, can include respiratory issues, allergic reactions, or complications with anesthesia administration.
- Specific risks of breast reconstruction
- Capsular contracture: Scar tissue may form around breast implants, leading to firmness, discomfort, or changes in breast shape.
- Implant rupture or leakage: Silicone or saline breast implants may rupture or leak, requiring implant removal or replacement.
- Delayed wound healing: Some individuals may experience delayed wound healing, which can lead to infection or other complications.
- Changes in sensation: Numbness, hypersensitivity, or changes in sensation in the breasts or nipples may occur, especially with nerve damage during surgery.
- Asymmetry: Achieving perfect symmetry between the reconstructed breast and the natural breast can be challenging and may require additional procedures.
- Scarring: Scarring is inevitable after surgery, and while efforts are made to minimize scarring, individual healing responses can vary.
- Long-term considerations:
- Revision surgery: Some individuals may require additional surgeries to optimize breast shape and symmetry, or address complications that arise over time.
- Psychological impact: Breast reconstruction surgery can have emotional implications, and some individuals may experience body image issues, anxiety, or depression postoperatively.
- Rare complications
- Seroma: Fluid accumulation around the surgical site.
- Hematoma: Collection of blood under the skin.
- Fat necrosis: Death of fat tissue in the reconstructed breast.
- Thrombosis: Blood clots in the deep veins, which can be a serious complication.
It is crucial to maintain open communication with your plastic surgeon, adhere to postoperative instructions, attend follow-up appointments, and promptly report any concerning symptoms or complications. By understanding the potential risks and complications associated with breast reconstruction surgery, you can make informed decisions and actively participate in your recovery process.
Cost and insurance coverage
The cost of breast reconstruction surgery can vary depending on several factors, including the type of reconstruction technique used, the surgeon's experience, the geographic location of the surgical facility, and any additional procedures or hospital fees involved. Here are some key points to consider regarding the cost and insurance coverage for breast reconstruction:
- Cost factors
- Type of reconstruction: The cost may differ based on whether you choose implant-based reconstruction or autologous tissue reconstruction.
- Surgeon's fees: The surgeon's fee typically includes their expertise, preoperative consultations, surgical procedures, and postoperative care.
- Hospital or facility fees: Costs associated with the surgical facility, operating room, anesthesia, medical supplies, and overnight stays (if required) can contribute to the overall cost.
- Additional procedures: If additional procedures, such as nipple reconstruction or symmetry procedures on the opposite breast, are performed, they may incur extra costs.
- Insurance coverage
- Federal law mandate: The Women's Health and Cancer Rights Act of 1998 mandates that health insurance plans that cover mastectomy must also cover breast reconstruction surgery.
- In-network providers: It is essential to check if your plastic surgeon and the surgical facility are in-network providers with your insurance plan to maximize coverage and minimize out-of-pocket costs.
- Preauthorization: Prior authorization from your insurance company may be necessary for breast reconstruction surgery. Your surgeon's office can assist in obtaining preauthorization and verifying coverage details.
- Out-of-pocket costs: While insurance typically covers a significant portion of breast reconstruction costs, you may still be responsible for deductibles, copayments, or coinsurance. It is crucial to review your insurance policy for coverage details and potential out-of-pocket expenses.
- Financial assistance
- Medicare and Medicaid: These programs may provide coverage for breast reconstruction surgery after mastectomy.
- Charitable organizations: Some nonprofit organizations offer financial assistance or grants to help individuals with the costs of breast reconstruction surgery.
- Payment plans: Surgical facilities or plastic surgery practices may offer payment plans or financing options to help manage the cost of breast reconstruction over time.
It is recommended to consult with your insurance provider to understand the specifics of your coverage, including deductibles, copayments, and any preauthorization requirements for breast reconstruction surgery.
By being informed about the cost factors, insurance coverage, and available financial assistance options, you can navigate the financial aspects of breast reconstruction surgery more effectively and make informed decisions about your treatment.
FAQs
Do reconstructed breasts have sensations?
While reconstructed breasts may not have the same level of sensation as natural breasts, many individuals report gradual improvements in sensation over time. It is important to have realistic expectations regarding sensation recovery and to communicate any concerns or changes in sensation with your plastic surgeon during follow-up appointments.
Is implant or flap breast reconstruction a better choice?
The choice between implant-based and flap (autologous tissue) breast reconstruction depends on individual factors such as body type, desired outcome, and personal preference. Implant reconstruction offers a shorter recovery time and less invasive surgery, while flap reconstruction provides a more natural look and feel but involves a longer recovery and more complex surgery.
How long does a breast reconstruction surgery take to complete?
Breast reconstruction surgery duration can vary based on the specific technique, complexity of the procedure, and whether it is performed in one stage or multiple stages. On average, the surgery can take approximately 2 to 6 hours, but more complex cases may require longer operating times.
Will a reconstructed breast look natural?
With advances in surgical techniques and materials, modern breast reconstruction procedures aim to achieve natural-looking results. While reconstructed breasts may not feel identical to natural breasts, skilled plastic surgeons can create aesthetically pleasing outcomes that closely resemble the appearance of a natural breast.